HTML
Perspective - (2022) Volume 12, Issue 3
A Short Note on Chemosensitization
Toshiyuka Suzuki**Correspondence: Toshiyuka Suzuki, Department of Pharmacy, Tokyo University of Pharmacy and Life Sciences, Hachioji, Tokyo, Japan, Email:
Received: 07-Feb-2022, Manuscript No. IJP-22-61746; Editor assigned: 11-Feb-2022, Pre QC No. IJP-22-61746 (PQ); Reviewed: 28-Feb-2022, QC No. IJP-22-61746; Revised: 04-Mar-2022, Manuscript No. IJP-22-61746 (R); Published: 11-Mar-2022, DOI: 10.37532/2249-1848-2022.12(3).15
Description
Chemosensitization is a cancer treatment method that involves using a medication to make tumour cells more susceptible to chemotherapeutic agents. The clinical usage of a chemosensitizer results in lower cytotoxic anticancer medication dosages, overcomes chemoresistance by tumour cells to these treatments, avoids toxicity to normal cells, and reduces anticancer drug side effects for the patient. Anticancer drug combinations can have synergistic, additive, or antagonistic effects depending on how they interact. The combination of anticancer and chemosensitizing drugs, on the other hand, produces primarily synergistic effects. Because the activity of ATP-binding cassette (ABC) proteins can reduce drug efficacy when stable levels of the active agent are required in the general circulation or in tumour tissue, researchers are working hard to develop novel, specific reversing agents for these pumps, which can be incorporated into the chemosensitizer concept.
Three generations of medications have resulted from the ongoing quest for molecules that act directly on ABC transporter proteins to limit their action. The calcium channel blocker verapamil and the immunomodulatory cyclosporine A, both of which can inhibit MDR1 but are poor substrates of this pump, were among the first wave of chemosensitizers. Both were successful in resensitizing MDR1- mediated drug resistant cancer cells in vitro. Despite entering clinical trials, these compounds were shown to be ineffective for cancer patients due to the large dose necessary and the side effects of combining them with verapamil or cyclosporine A. A second generation of MDR1 modulators was created in an attempt to improve positive qualities while reducing negative effects. The most promising of these was SDZ PSC833 or valspodar, a cyclosporine A analogue. This medicine is 10 to 20 times more effective at reducing MDR1 activity, but it comes with more substantial side effects. Valspodar treatment resulted in individuals being overexposed to cytotoxic medication serum concentrations, according to clinical trials. LY335979 (zosuquidar), GF12918 (elacridar), CBT-1, and XR9576 are examples of thirdgeneration chemosensitizers (tariquidar). These are highly effective even at nanomolar concentrations and show promise when compared to previous generations' results. Surprisingly, these ABC modulators are less hazardous and have no effect on anticancer medication pharmacokinetics. The specificity of these medications is one of their distinct advantages. For example, zosuquidar has a strong efficacy in inhibiting MDR1 (Ki of around 60 nM), but has little effect on MRPs or BCRP.
Chemosensitization can also be accomplished by increasing the amount of medication absorbed by tumour cells. In addition to the previously mentioned way of achieving this goal by medication targeting, there is also the option of restoring or enhancing the expression or function of naturally occurring carriers implicated in this process. To demonstrate these possibilities, consider the copper transporter CTR1, which is a primary influx transporter for platinum medicines. Thus, in a mouse model of human cervical cancer, combining cisplatin with a copper chelator improves CTR1 availability for cisplatin uptake, resulting in increased cisplatin-DNA adduct levels in malignant but not normal tissues, reduced angiogenesis, and improved therapeutic efficiency. Furthermore, cisplatin has been shown to inhibit CTR1 expression by stimulating proteasomal degradation of this drug carrier, limiting the ability of tumour cells to absorb it. Bortezomib, a proteasomal inhibitor, inhibits cisplatin-induced CTR1 degradation, increasing the abundance of transporter proteins at the plasma membrane of ovarian cancer cells as well as their ability to take up cisplatin, leading to increased apoptosis activation.
Manuscript Submission
Submit your manuscript at Online Submission System
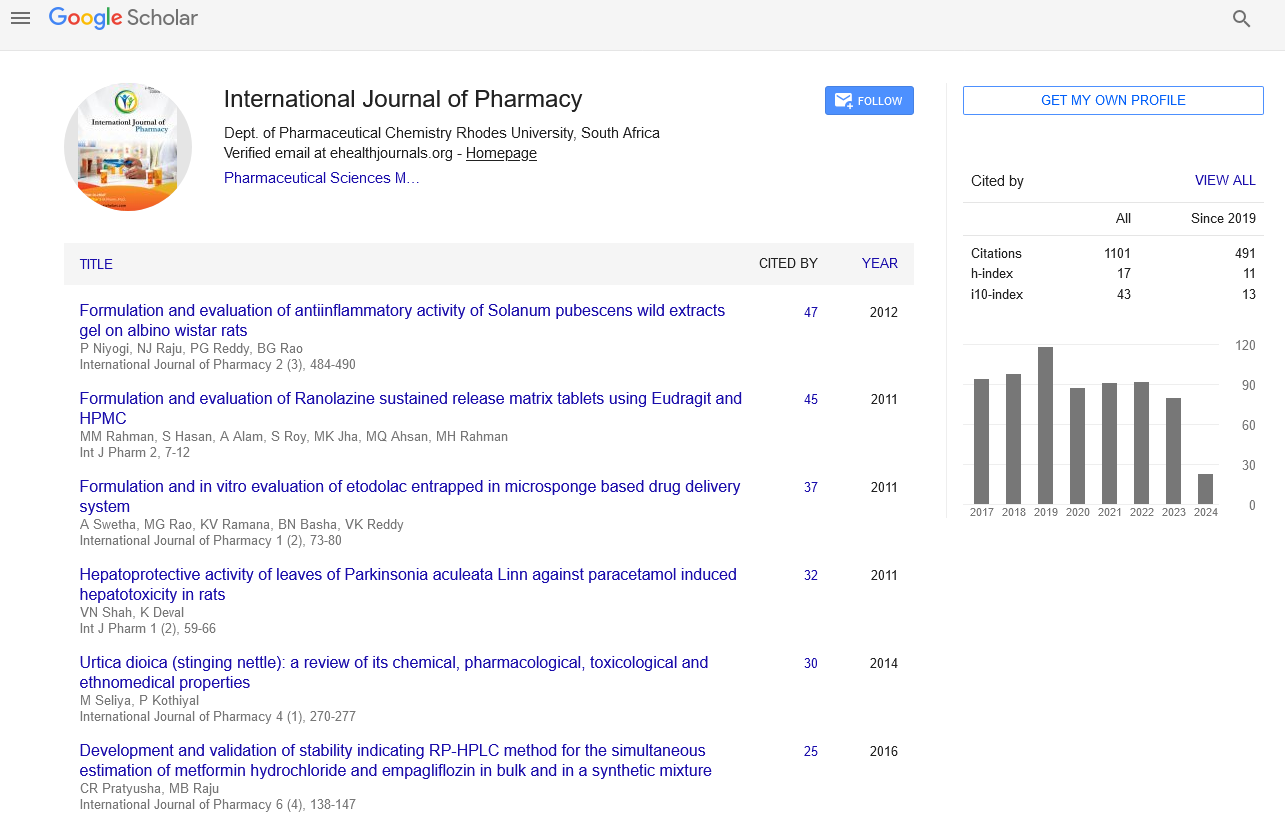
Google scholar citation report
Citations : 1101
International Journal of Pharmacy received 1101 citations as per google scholar report
International Journal of Pharmacy peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- HINARI
- Index Copernicus
- Google Scholar
- The Global Impact Factor (GIF)
- Polish Scholarly Bibliography (PBN)
- Cosmos IF
- Open Academic Journals Index (OAJI)
- Directory of Research Journal Indexing (DRJI)
- EBSCO A-Z
- OCLC- WorldCat
- MIAR
- International committee of medical journals editors (ICMJE)
- Scientific Indexing Services (SIS)
- Scientific Journal Impact Factor (SJIF)
- Euro Pub
- Eurasian Scientific Journal Index
- Root indexing
- International Institute of Organized Research
- InfoBase Index
- International Innovative Journal Impact Factor
- J-Gate