HTML
Commentary - (2024) Volume 14, Issue 3
Antifungal Medications and their Mechanisms, Classification, Indications and Challenges
Jurun Mclean**Correspondence: Jurun Mclean, Department of Pharmacy, University of London, London, UK, Email:
Received: 21-Apr-2024, Manuscript No. IJP-24-137601; Editor assigned: 24-Apr-2024, Pre QC No. IJP-24-137601 (PQ); Reviewed: 14-May-2024, QC No. IJP-24-137601; Revised: 22-May-2024, Manuscript No. IJP-24-137601 (R); Published: 29-May-2024, DOI: 10.37522/2249-1848.2024.14(3).114
About the Study
Antifungal medications, also known as antimitotic agents, are drugs used to treat fungal infections. These infections can range from superficial, affecting the skin, nails, or hair, to systemic, impacting internal organs and tissues. Fungal infections are caused by a variety of fungi, including yeasts, molds, and dermatophytes. Effective antifungal treatment is essential for managing these infections, particularly in immuno compromised individuals.
Classification of antifungal medications
Antifungal medications are broadly classified based on their chemical structure and mechanism of action. The main classes include:
Polyenes: This class includes drugs like amphotericin B and nystatin. Polyenes bind to ergosterol, a critical component of fungal cell membranes, creating pores that lead to cell death. Amphotericin B is often reserved for severe systemic infections due to its potential toxicity, particularly nephrotoxicity.
Azoles: Azole antifungals are subdivided into imidazoles (e.g., ketoconazole) and triazoles (e.g., fluconazole, itraconazole, voriconazole). These drugs inhibit the synthesis of ergosterol by blocking the enzyme lanosterol 14-alpha-demethylase, disrupting cell membrane formation. Azoles are widely used due to their broad spectrum of activity and oral bioavailability.
Echinocandins: Including drugs such as caspofungin, micafungin, and anidulafungin, echinocandins inhibit the synthesis of β-glucan, an essential component of the fungal cell wall. These drugs are particularly effective against Candida species and are well-tolerated with minimal side effects.
Allylamines: Terbinafine, the most well-known allylamine, inhibits squalene epoxidase, another enzyme in the ergosterol synthesis pathway. It is primarily used for dermatophyte infections, such as tinea pedis (athlete’s foot) and onychomycosis (fungal nail infection).
Pyrimidine analogues: Flucytosine is converted within fungal cells to fluorouracil, which inhibits DNA and RNA synthesis. It is typically used in combination with other antifungals like amphotericin B to treat severe infections like cryptococcal meningitis.
Indications and uses
Antifungal medications are prescribed based on the type and severity of the fungal infection:
Superficial infections: Topical antifungals such as clotrimazole and miconazole are commonly used for skin and mucosal infections like athlete’s foot, ringworm, and vaginal candidiasis. For nail infections, oral terbinafine or itraconazole may be prescribed due to the difficulty of eradicating the infection topically.
Systemic infections: For more severe infections, especially in immunocompromised patients (e.g., those with HIV/AIDS, cancer patients, or organ transplant recipients), systemic antifungals are necessary. Fluconazole is often used for systemic candidiasis, while voriconazole and amphotericin B are choices for invasive aspergillosis
and other serious infections.
Resistance and challenges
The emergence of antifungal resistance is a growing concern. Overuse and misuse of antifungals have led to resistant strains of Candida and Aspergillus. Candida auris, for example, is a multi-drug resistant fungus that poses a significant threat in healthcare settings. To combat resistance, antifungal stewardship programs promote the appropriate use of these medications.
Side effects and toxicity
Antifungal medications can have significant side effects, particularly with prolonged use:
Polyenes: Amphotericin B can cause nephrotoxicity, electrolyte imbalances, and infusion-related reactions. Liposomal formulations have been developed to reduce toxicity.
Azoles: These can cause hepatotoxicity, gastrointestinal disturbances, and drug interactions due to their inhibition of cytochrome P450 enzymes.
Echinocandins: Generally well-tolerated but can cause mild liver enzyme elevations and infusion-related reactions.
Allylamines: Terbinafine can cause gastrointestinal symptoms, liver enzyme elevation, and, rarely, hepatotoxicity.
Pyrimidine analogues: Flucytosine may cause bone marrow suppression and gastrointestinal issues, necessitating regular blood monitoring.
Future directions
Ongoing research aims to develop new antifungal agents with better efficacy, reduced toxicity, and lower potential for resistance. Innovations include novel drug formulations, combination therapies and agents targeting new fungal pathways. Additionally, advancements in diagnostics can help in the early and accurate identification of fungal infections, allowing for timely and targeted treatment.
Conclusion
In conclusion, antifungal medications play a critical role in managing fungal infections. While they have transformed the treatment landscape, challenges such as resistance and toxicity highlight the need for continued research and judicious use of these vital drugs. Their continued development and appropriate use are essential for managing the diverse and potentially severe manifestations of fungal diseases, ensuring improved health outcomes and quality of life for affected individuals.Manuscript Submission
Submit your manuscript at Online Submission System
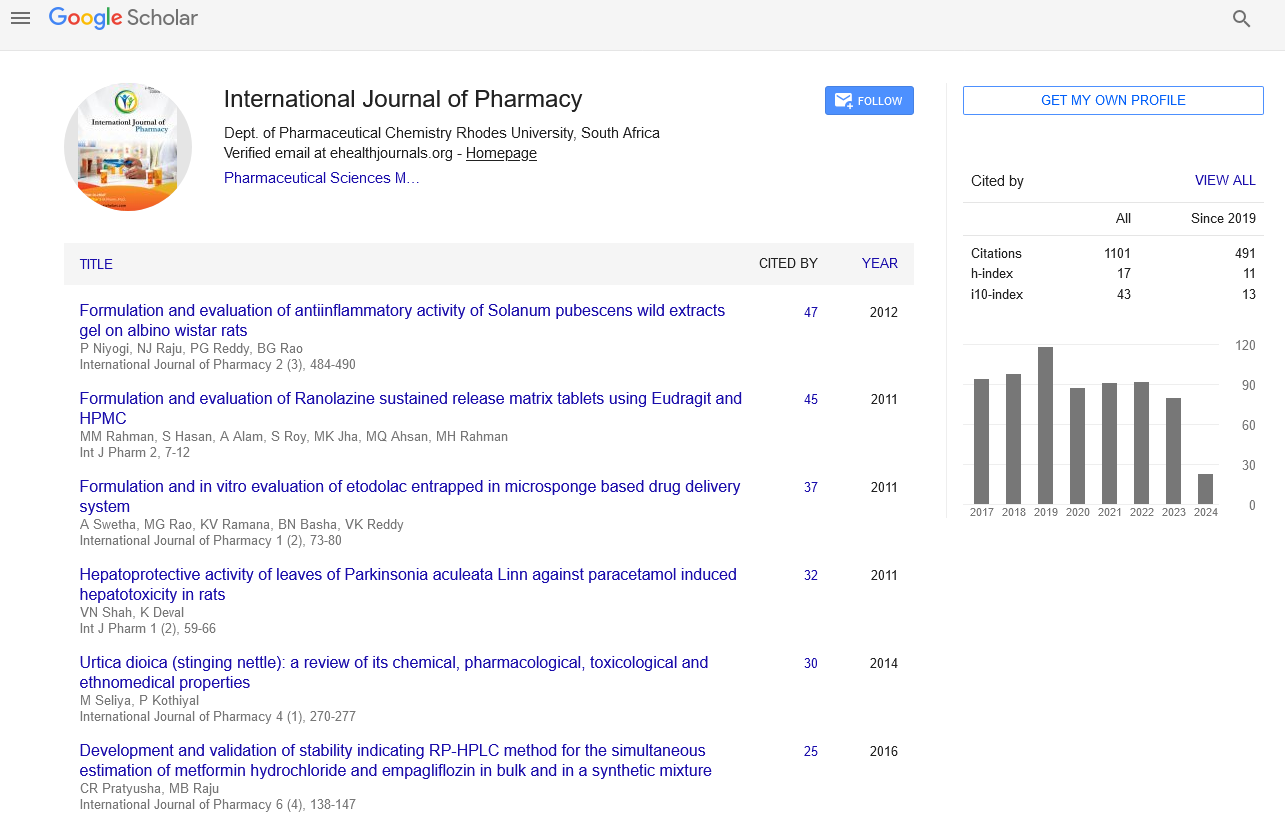
Google scholar citation report
Citations : 1101
International Journal of Pharmacy received 1101 citations as per google scholar report
International Journal of Pharmacy peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- HINARI
- Index Copernicus
- Google Scholar
- The Global Impact Factor (GIF)
- Polish Scholarly Bibliography (PBN)
- Cosmos IF
- Open Academic Journals Index (OAJI)
- Directory of Research Journal Indexing (DRJI)
- EBSCO A-Z
- OCLC- WorldCat
- MIAR
- International committee of medical journals editors (ICMJE)
- Scientific Indexing Services (SIS)
- Scientific Journal Impact Factor (SJIF)
- Euro Pub
- Eurasian Scientific Journal Index
- Root indexing
- International Institute of Organized Research
- InfoBase Index
- International Innovative Journal Impact Factor
- J-Gate