HTML
Perspective - (2024) Volume 14, Issue 2
Assessing Low and High-Dose Calcium Supplements and Preeclampsia Risk: Identifying the Clinical Consequences
Robert Benjamin**Correspondence: Robert Benjamin, Department of Pharmacy, University of Berlin, Berlin, Germany, Email:
Received: 20-Feb-2024, Manuscript No. IJP-24-130552; Editor assigned: 23-Feb-2024, Pre QC No. IJP-24-130552 (PQ); Reviewed: 08-Mar-2024, QC No. IJP-24-130552; Revised: 15-Mar-2024, Manuscript No. IJP-24-130552 (R); Published: 22-Mar-2024, DOI: 10.37522/2249-1848.2024.14(2).102
About the Study
Preeclampsia, a hypertensive disorder unique to pregnancy, poses significant risks to maternal and fetal health worldwide. Characterized by elevated blood pressure and proteinuria after 20 weeks of gestation, preeclampsia remains a leading cause of maternal and perinatal morbidity and mortality. While the etiology of this condition is multifactorial and not fully understood, emerging research suggests that calcium supplementation may play a crucial role in its prevention. However, debates persist regarding the optimal dosage of calcium supplementation to mitigate the risk of preeclampsia. This article delves into the ongoing discourse surrounding low- versus high-dose calcium supplements and their impact on the risk of preeclampsia.
Historically, studies have demonstrated a potential link between calcium intake and the incidence of preeclampsia. The landmark WHO Calcium Supplementation Trial Group's study in 1997 provided initial evidence supporting calcium supplementation's protective effect against preeclampsia. Subsequent meta-analyses and Randomized Controlled Trials (RCTs) further corroborated these findings, leading to the integration of calcium supplementation into antenatal care protocols worldwide.
However, the optimal dosage of calcium remains a subject of contention among researchers and clinicians. Proponents of lowdose calcium supplementation argue for its cost-effectiveness and minimal adverse effects. Low-dose regimens typically involve daily calcium supplementation ranging from 500 to 1000 mg elemental calcium. Advocates highlight the accessibility and affordability of low-dose supplements, particularly in resource-limited settings where preeclampsia poses a considerable burden.
Furthermore, studies have suggested that even modest increases in calcium intake may confer protective benefits against preeclampsia, making low-dose supplementation an attractive option for widespread implementation. Conversely, proponents of high-dose calcium supplementation advocate for its potentially enhanced efficacy in preventing preeclampsia.
High-dose regimens typically involve daily calcium supplementation exceeding 1500 mg elemental calcium. Advocates point to evidence suggesting a dose-response relationship between calcium intake and preeclampsia risk reduction. High-dose supplementation may more effectively address the underlying pathophysiological mechanisms implicated in preeclampsia, such as endothelial dysfunction and abnormal placental perfusion. Additionally, some studies have proposed that high-dose calcium supplementation could yield secondary benefits, such as reducing the risk of preterm birth and low birth weight.
Despite these arguments, the optimal dosage of calcium supplementation for preventing preeclampsia remains elusive, with conflicting evidence complicating clinical decision-making. Several RCTs comparing low- versus high-dose calcium supplementation have yielded inconsistent results, further fueling the debate. Factors such as variations in study populations, calcium formulations, and adherence rates contribute to the heterogeneity of findings across trials.
Moreover, the efficacy of calcium supplementation may be influenced by individual patient characteristics, including baseline dietary calcium intake, gestational age at initiation, and comorbidities such as obesity and chronic hypertension. These complexities underscore the need for personalized approaches to calcium supplementation during pregnancy, taking into account the unique risk profiles of expectant mothers.
Moving forward, future research endeavors should prioritize elucidating the mechanistic underpinnings of calcium's role in preeclampsia pathogenesis, as well as identifying subpopulations that may derive the greatest benefit from supplementation. Additionally, well-designed RCTs with rigorous methodology and long-term follow-up are warranted to definitively establish the optimal dosage and timing of calcium supplementation.
In the interim, clinicians must navigate the existing evidence landscape to inform individualized patient care decisions. Shared decision-making between healthcare providers and pregnant individuals should weigh the potential benefits and risks of calcium supplementation, considering factors such as cost, tolerability, and patient preferences. Furthermore, comprehensive antenatal care should encompass a comprehensive approach to preeclampsia prevention, incorporating strategies beyond calcium supplementation, such as regular blood pressure monitoring, adequate nutrition, and early detection of risk factors.
In conclusion, the debate surrounding low versus high-dose calcium supplementation for preventing preeclampsia reflects the complexity of maternal-fetal health interventions. While both approaches offer theoretical benefits, uncertainties persist regarding their comparative efficacy and safety. Continued research efforts and clinical vigilance are essential to optimize preeclampsia prevention strategies and improve maternal and perinatal outcomes worldwide.
Manuscript Submission
Submit your manuscript at Online Submission System
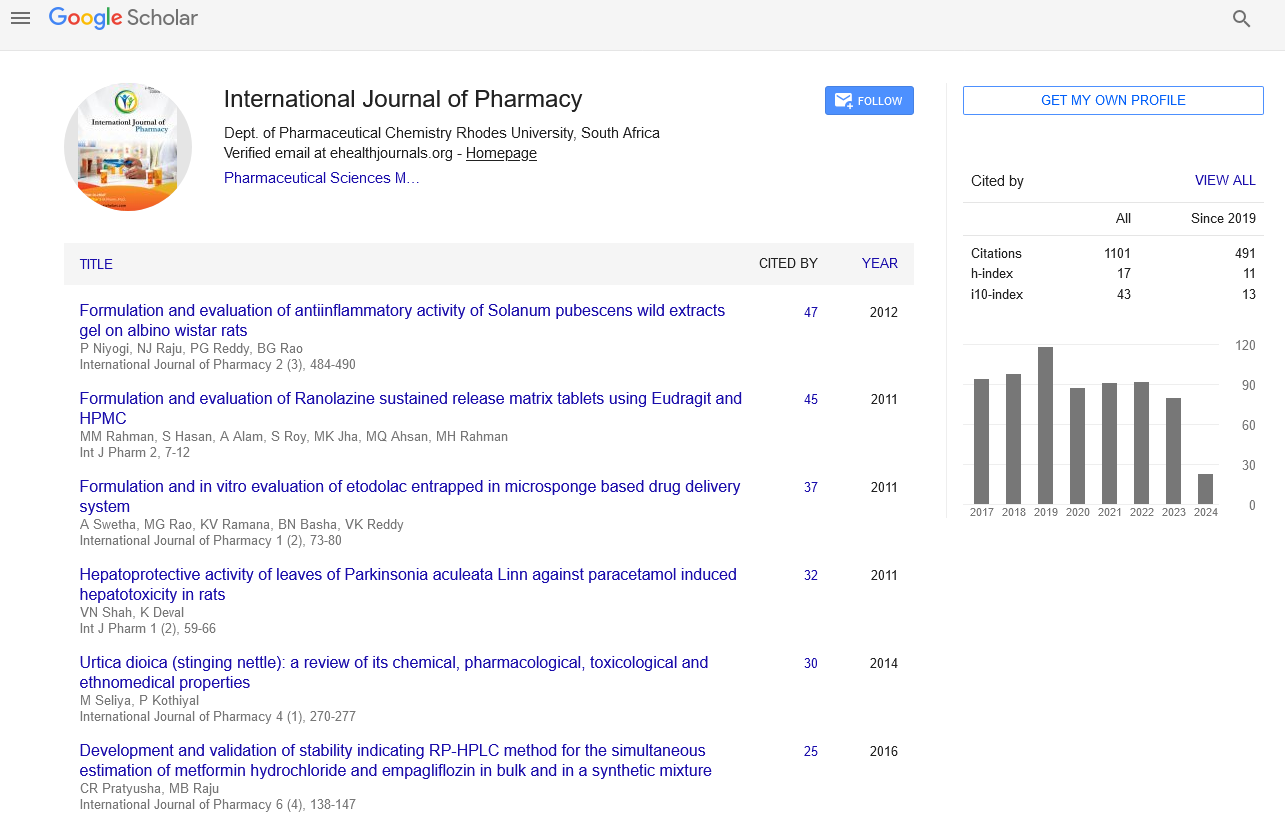
Google scholar citation report
Citations : 1101
International Journal of Pharmacy received 1101 citations as per google scholar report
International Journal of Pharmacy peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- HINARI
- Index Copernicus
- Google Scholar
- The Global Impact Factor (GIF)
- Polish Scholarly Bibliography (PBN)
- Cosmos IF
- Open Academic Journals Index (OAJI)
- Directory of Research Journal Indexing (DRJI)
- EBSCO A-Z
- OCLC- WorldCat
- MIAR
- International committee of medical journals editors (ICMJE)
- Scientific Indexing Services (SIS)
- Scientific Journal Impact Factor (SJIF)
- Euro Pub
- Eurasian Scientific Journal Index
- Root indexing
- International Institute of Organized Research
- InfoBase Index
- International Innovative Journal Impact Factor
- J-Gate