HTML
Opinion - (2024) Volume 14, Issue 4
Bridging Genetics and Pharmacology for Personalized Treatment through Pharmacogenomics
Rajesh Verma**Correspondence: Rajesh Verma, Department of Pharmaceutical Biotechnology, National Institute of Pharmaceutical Education and Research, Guwahati, India, Email:
Received: 01-Jul-2024, Manuscript No. IJP-24-141385; Editor assigned: 04-Jul-2024, Pre QC No. IJP-24-141385(PQ); Reviewed: 18-Jul-2024, QC No. IJP-24-141385; Revised: 25-Jul-2024, Manuscript No. IJP-24-141385(R); Published: 31-Jul-2024, DOI: 10.37522/2249-1848.2024.14(4).116
About the Study
Pharmacogenomics, an interdisciplinary field combining genetics and pharmacology, has emerged as a revolutionary approach to tailor medical treatments to individual genetic profiles. This article describes the foundational principles of pharmacogenomics, its practical applications across various medical specialties, challenges faced in implementation, and future prospects for enhancing personalized medicine. Pharmacogenomics represents a pivotal shift in healthcare towards precision medicine, where treatment decisions are guided by an individual's genetic makeup rather than a one-size-fits-all approach. By elucidating how genetic variations influence drug response, pharmacogenomics aims to optimize therapeutic efficacy, minimize adverse effects, and improve patient outcomes. This article searches into the mechanisms underlying pharmacogenomics, its clinical applications, and the ongoing efforts to integrate genetic testing into routine clinical practice. At its core, pharmacogenomics investigates how genetic variations affect an individual's response to drugs. Variants in genes encoding drug-metabolizing enzymes, transporters, and drug targets can significantly influence pharmacokinetics and pharmacodynamics. For example, polymorphisms in the CYP2D6 gene alter the metabolism of various drugs, impacting treatment efficacy and toxicity profiles. Understanding these genetic variations allows healthcare providers to personalize drug therapy, ensuring optimal outcomes tailored to each patient's genetic profile. Pharmacogenomics has diverse applications across medical specialties, including oncology, psychiatry, cardiology, and infectious diseases. In oncology, genetic testing helps identify patients who are likely to respond to specific chemotherapy agents, enabling oncologists to prescribe the most effective treatments while minimizing unnecessary toxicity. Similarly, in psychiatry, genetic insights inform the selection of antidepressants or antipsychotics based on individual genetic profiles, enhancing treatment efficacy and reducing adverse effects. Integration of pharmacogenomic testing into clinical practice is exemplified in areas such as cardiovascular medicine, where genetic variants influence responses to drugs like clopidogrel (antiplatelet agent) and statins (lipid-lowering drugs). Tailoring drug doses based on genetic information enhances therapeutic outcomes and reduces the risk of adverse reactions, thereby optimizing patient care.
Despite its potential, pharmacogenomics confronts certain obstacles that impede its extensive integration into clinical practice. Numerous genetic variations have subtle impacts on medication response that are still poorly understood, making the interpretation of genetic data challenging. Pharmacogenomic testing implementation presents logistical and budgetary challenges in healthcare settings since it requires a strong infrastructure for genetic testing, data processing, clinical decision support systems. Integrating pharmacogenomics into clinical care is also impacted by ethical issues, such as informed permission, patient confidentiality, and possible consequences for employment and insurance coverage. In order to provide fair access to pharmacogenomic technologies and safeguard patient rights, it is imperative to address these ethical, legal, and societal ramifications. Through advances in technology and cooperative research efforts, pharmacogenomics has the potential to advance personalised medicine in the future. The accuracy and accessibility of pharmacogenomic testing will be improved by ongoing developments in genomic sequencing technology and bioinformatics tools, making it more practical for routine clinical usage. Integration of artificial intelligence and machine learning algorithms will further refine the interpretation of complex genetic data, empowering healthcare providers to make data-driven decisions in real-time. Research initiatives focusing on diverse patient populations and underrepresented groups are essential for developing inclusive pharmacogenomic guidelines that reflect genetic diversity. Collaboration between researchers, clinicians, pharmaceutical companies, and regulatory agencies is pivotal in translating pharmacogenomic discoveries into actionable clinical practices.
Education and training programs are crucial for equipping healthcare providers with the knowledge and skills necessary to integrate pharmacogenomic information into patient care effectively. Public awareness campaigns and patient education initiatives will promote understanding of the benefits and implications of pharmacogenomics testing, fostering informed decision-making and patient engagement in personalized medicine. Pharmacogenomics represents a transformative approach to healthcare, enabling personalized drug therapy based on individual genetic profiles. While challenges exist, ongoing research and many technological advancements are tiling way for pharmacogenomics to become an integral part of clinical practice. By using genetic insights to optimize drug efficacy and safety, pharmacogenomics holds the potential to revolutionize patient care, improve treatment outcomes, and usher in a new era of precision medicine.
Manuscript Submission
Submit your manuscript at Online Submission System
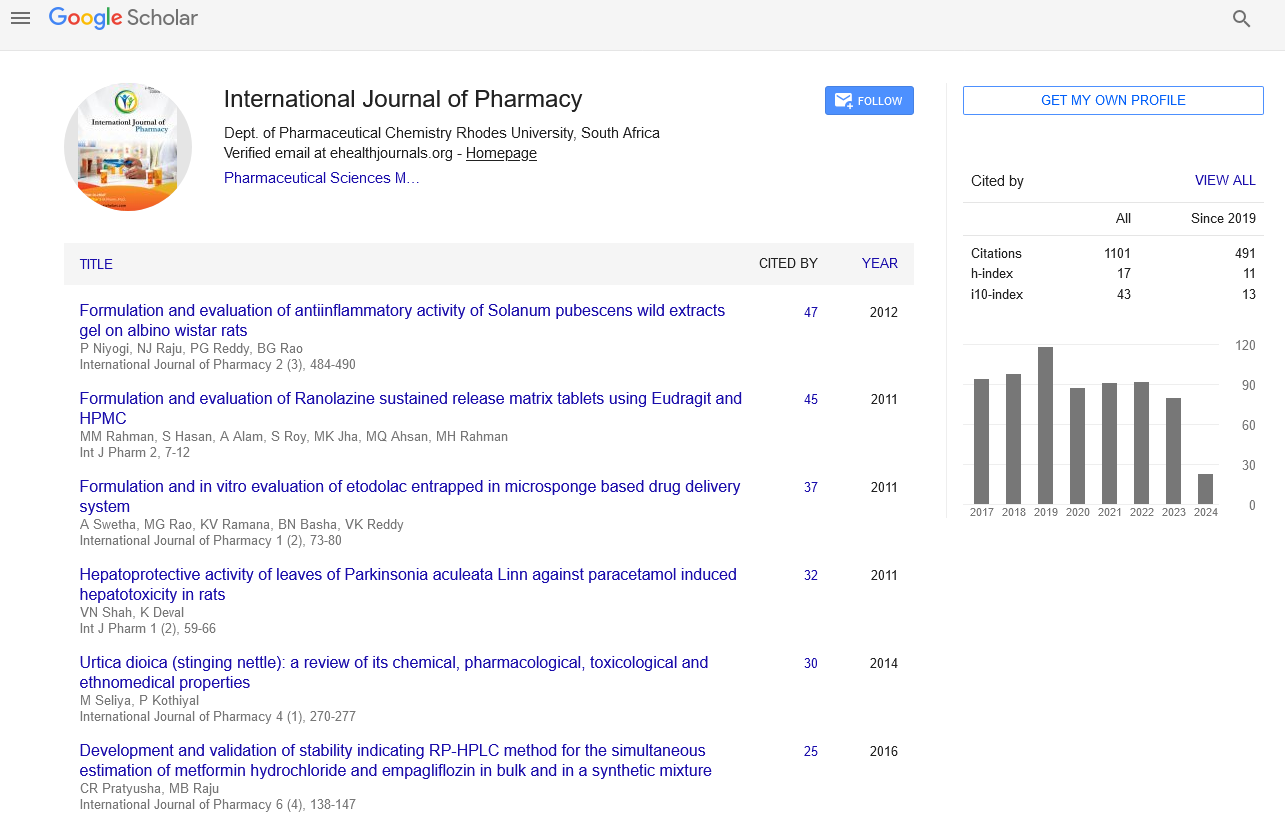
Google scholar citation report
Citations : 1101
International Journal of Pharmacy received 1101 citations as per google scholar report
International Journal of Pharmacy peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- HINARI
- Index Copernicus
- Google Scholar
- The Global Impact Factor (GIF)
- Polish Scholarly Bibliography (PBN)
- Cosmos IF
- Open Academic Journals Index (OAJI)
- Directory of Research Journal Indexing (DRJI)
- EBSCO A-Z
- OCLC- WorldCat
- MIAR
- International committee of medical journals editors (ICMJE)
- Scientific Indexing Services (SIS)
- Scientific Journal Impact Factor (SJIF)
- Euro Pub
- Eurasian Scientific Journal Index
- Root indexing
- International Institute of Organized Research
- InfoBase Index
- International Innovative Journal Impact Factor
- J-Gate