HTML
Opinion Article - (2024) Volume 14, Issue 3
Clinical Data Management in Pharmaceuticals and Advancements in Technology
Angelo Mathews**Correspondence: Angelo Mathews, Department of Pharmacy, University of Milan, Milan, Italy, Email:
Received: 22-Apr-2024, Manuscript No. IJP-24-137596; Editor assigned: 25-May-2024, Pre QC No. IJP-24-137596 (PQ); Reviewed: 09-May-2024, QC No. IJP-24-137596; Revised: 16-May-2024, Manuscript No. IJP-24-137596 (R); Published: 24-May-2024, DOI: 10.37522/2249-1848.2024.14(3).110
About the Study
Clinical Data Management (CDM) is an important aspect of the pharmaceutical industry, ensuring that data collected during clinical trials is accurate, reliable, and secure. The process encompasses the planning, collection, cleaning, and analysis of data, ultimately leading to the generation of high-quality datasets essential for regulatory approval and subsequent market release of new drugs. This field has seen significant advancements, driven by the need for efficiency, accuracy, and compliance with stringent regulatory requirements.
The importance of clinical data management
CDM plays a vital role in the drug development process. Highquality data is essential for making informed decisions about the efficacy and safety of new drugs. Poorly managed data can lead to incorrect conclusions, regulatory delays, and increased costs. Effective CDM ensures that data integrity is maintained throughout the trial, from initial data collection to the final analysis.
Components of clinical data management
Data collection
Data collection begins with the design of Case Report Forms (CRFs), which are used to capture all necessary data points from clinical trial participants. Electronic Data Capture (EDC) systems have largely replaced paper-based CRFs, providing more accurate and real-time data collection.
Data cleaning
Data cleaning involves identifying and correcting errors or inconsistencies in the collected data. This process is critical to ensure that the dataset is accurate and reliable. Common cleaning methods include range checks, consistency checks, and validation rules.
Data integration
Clinical trials often generate diverse data types, including laboratory results, imaging data, and patient-reported outcomes. Integrating these various data sources into a cohesive dataset is crucial for comprehensive analysis. After data cleaning and integration, the database is "locked," meaning no further changes can be made. This final dataset is then used for statistical analysis and regulatory submission.
Advances in clinical data management
Electronic Data Capture (EDC) systems: EDC systems have revolutionized CDM by enabling real-time data entry, reducing transcription errors, and enhancing data accuracy. These systems provide secure, cloud-based platforms that facilitate remote data entry and monitoring.
Data standardization: The adoption of standardized data formats, such as those recommended by the Clinical Data Interchange Standards Consortium (CDISC), has improved data interoperability and sharing. Standardization ensures that data from different sources can be seamlessly integrated and compared.
Artificial Intelligence (AI) and Machine Learning (ML): AI and ML technologies are increasingly being used to enhance data cleaning and analysis processes. These technologies can identify patterns and anomalies in large datasets, improving data quality and accelerating the analysis phase.
Block chain technology: Block chain technology offers a secure and transparent way to manage clinical trial data. By providing a tamperproof ledger of data transactions, block chain can enhance data integrity and traceability, addressing issues related to data fraud and manipulation.
Real-World Data (RWD) and Real-World Evidence (RWE): The integration of RWD and RWE into CDM practices is becoming more prevalent. These data sources provide insights into how drugs perform in real-world settings, complementing data from controlled clinical trials and enhancing the overall understanding of a drug's efficacy and safety.
Regulatory considerations
Regulatory agencies such as the FDA and EMA have stringent requirements for data management in clinical trials. Compliance with these regulations is essential to ensure that data is robust and reliable. Key regulatory guidelines include.
Good Clinical Practice (GCP): GCP guidelines set the standard for the design, conduct, monitoring, and reporting of clinical trials. Adherence to GCP ensures that the rights, safety, and well-being of trial participants are protected and that trial data is credible.
CFR part 11: This FDA regulation outlines the criteria for electronic records and electronic signatures. Compliance with 21 CFR part 11 ensures that electronic data is trustworthy and reliable.
Challenges and future directions
Despite advancements, CDM faces ongoing challenges such as managing large volumes of data, ensuring data privacy, and maintaining regulatory compliance. Looking ahead, the future of CDM will likely involve greater automation, enhanced data analytics, and increased use of decentralized trial designs. These innovations promise to streamline the CDM process, improve data quality, and accelerate the development of new pharmaceuticals.
Conclusion
In conclusion, clinical data management is a constantly developing field critical to the success of pharmaceutical development. Advances in technology, data standardization, and regulatory frameworks are enhancing the efficiency and accuracy of CDM, ultimately contributing to the delivery of safe and effective medicines to the market.Manuscript Submission
Submit your manuscript at Online Submission System
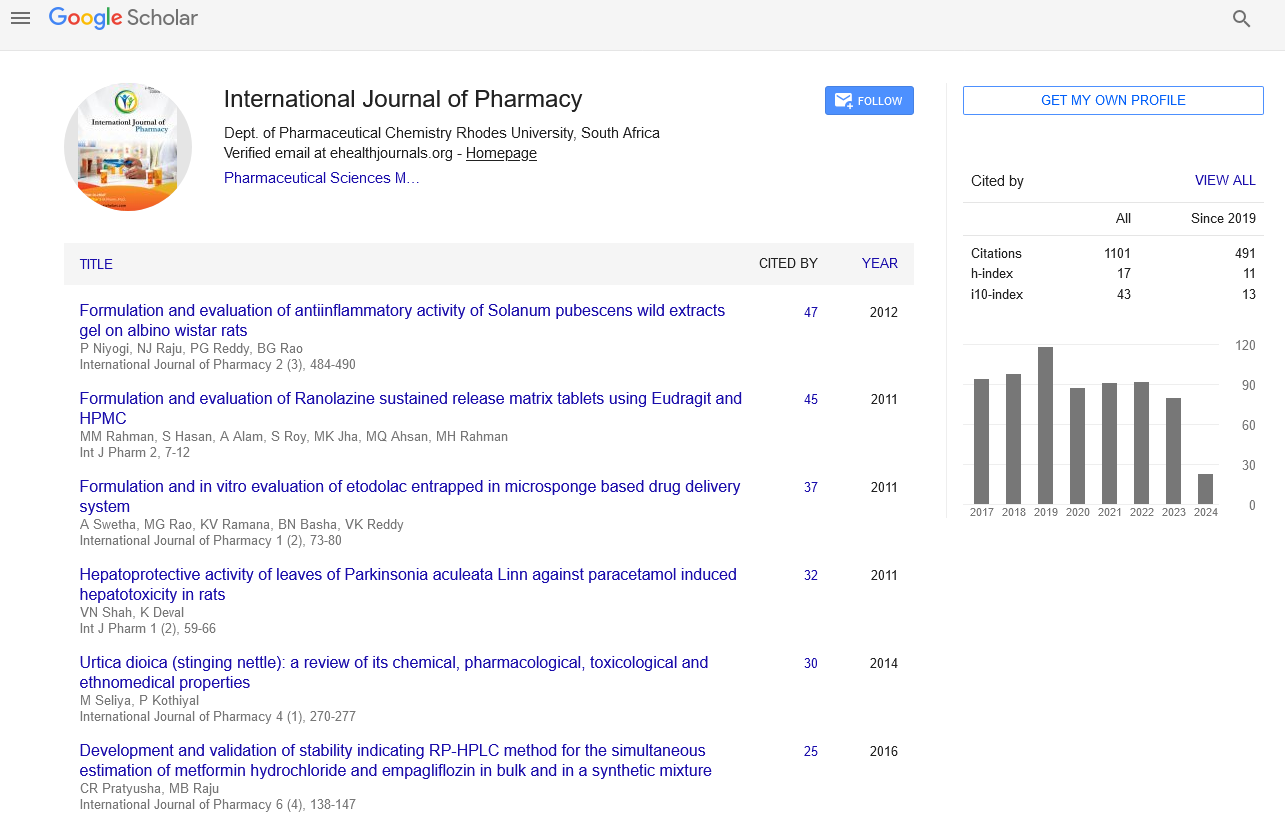
Google scholar citation report
Citations : 1101
International Journal of Pharmacy received 1101 citations as per google scholar report
International Journal of Pharmacy peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- HINARI
- Index Copernicus
- Google Scholar
- The Global Impact Factor (GIF)
- Polish Scholarly Bibliography (PBN)
- Cosmos IF
- Open Academic Journals Index (OAJI)
- Directory of Research Journal Indexing (DRJI)
- EBSCO A-Z
- OCLC- WorldCat
- MIAR
- International committee of medical journals editors (ICMJE)
- Scientific Indexing Services (SIS)
- Scientific Journal Impact Factor (SJIF)
- Euro Pub
- Eurasian Scientific Journal Index
- Root indexing
- International Institute of Organized Research
- InfoBase Index
- International Innovative Journal Impact Factor
- J-Gate