HTML
Perspective Article - (2023) Volume 13, Issue 3
Clinical Manifestations of Chronic Kidney Disease in Leptospirosis
Lindsey Miller**Correspondence: Lindsey Miller, Department of Pharmacy, University of Sao Paulo, Butanta, Sao Paulo, Brazil, Email:
Received: 03-Apr-2023, Manuscript No. IJP-23-100968; Editor assigned: 05-Apr-2023, Pre QC No. IJP-23-100968(PQ); Reviewed: 24-Apr-2023, QC No. IJP-23-100968; Revised: 03-May-2023, Manuscript No. IJP-23-100968(R); Published: 12-May-2023, DOI: 10.37532/2249-1848.2023.13(3).48
About the Study
A Chronic Kidney Disease (CKD) is a serious condition that affects millions of people worldwide, and it can have various underlying causes. One of the lesser-known causes of CKD is leptospirosis, a bacterial infection caused by the spirochete bacteria. Leptospirosis primarily spreads through contact with water contaminated by the urine of infected animals, such as rodents or livestock. The relationship between leptospirosis and CKD is complex and not yet fully understood. While leptospirosis is typically associated with Acute Kidney Injury (AKI) or acute renal failure, some individuals may progress to develop chronic kidney damage. This progression to CKD can occur due to several factors, including the severity of the initial infection, delayed or inadequate treatment, or certain host factors that predispose individuals to kidney damage.
In leptospirosis-associated CKD, the kidneys undergo persistent inflammation and scarring, leading to a gradual decline in kidney function over time. The exact mechanisms by which leptospira bacteria cause chronic kidney damage are still under investigation, but it is believed to involve a combination of direct invasion of renal tissues, immune system-mediated injury, and prolonged immune activation. The clinical manifestations of CKD in leptospirosis can vary widely, ranging from mild kidney dysfunction to End-Stage Renal Disease (ESRD) requiring dialysis or kidney transplantation. Patients may experience symptoms such as fatigue, decreased urine output, fluid retention, hypertension, and electrolyte imbalances. Early detection and intervention are crucial to slow the progression of CKD and prevent further kidney damage.
Managing CKD in leptospirosis involves a comprehensive approach that includes treating the underlying infection with appropriate antibiotics, managing complications such as hypertension and electrolyte imbalances, and implementing strategies to preserve renal function. When leptospirosis progresses to affect the kidneys, it can lead to a condition known as Leptospirosis-associated Kidney Disease or Leptospirosisinduced Acute Kidney Injury (AKI). In some individuals, particularly those with certain risk factors or prolonged exposure to the bacteria, this AKI can evolve into chronic kidney disease. The mechanisms by which leptospirosis contributes to the development of CKD are not fully understood, but there are several possible pathways. The bacteria can directly damage the kidney tissues, leading to inflammation and scarring. Additionally, the immune response triggered by the infection can cause an overactive immune reaction, resulting in further damage to the kidneys. Furthermore, leptospirosis can lead to cardiovascular complications, such as high blood pressure, which can contribute to the progression of kidney disease.
Early detection and prompt treatment of leptospirosis are crucial in preventing the development of CKD. Antibiotics such as doxycycline or penicillin are commonly prescribed to eliminate the bacteria. However, in cases where kidney function is already compromised, supportive care such as hydration and dialysis may be necessary to manage the kidney damage. Prevention plays a vital role in reducing the incidence of leptospirosis and its associated complications. Measures such as avoiding contact with contaminated water or soil, practicing good hygiene, wearing protective clothing, and vaccinating high-risk individuals, such as farmers or individuals in endemic areas, are essential in preventing leptospirosis infections. This involves adopting measures to minimize exposure to contaminated water sources, practicing good hygiene, wearing protective clothing in high-risk environments, and controlling rodent populations in urban and rural areas.
Conclusion
Understanding the underlying mechanisms and risk factors associated with leptospirosis-related CKD is vital for early detection, timely intervention, and implementing effective preventive strategies. Continued research and public health efforts are necessary to improve our understanding of this condition and reduce its burden on affected individuals and communities. Prevention plays a crucial role in reducing the incidence of leptospirosis and its associated complications.
Manuscript Submission
Submit your manuscript at Online Submission System
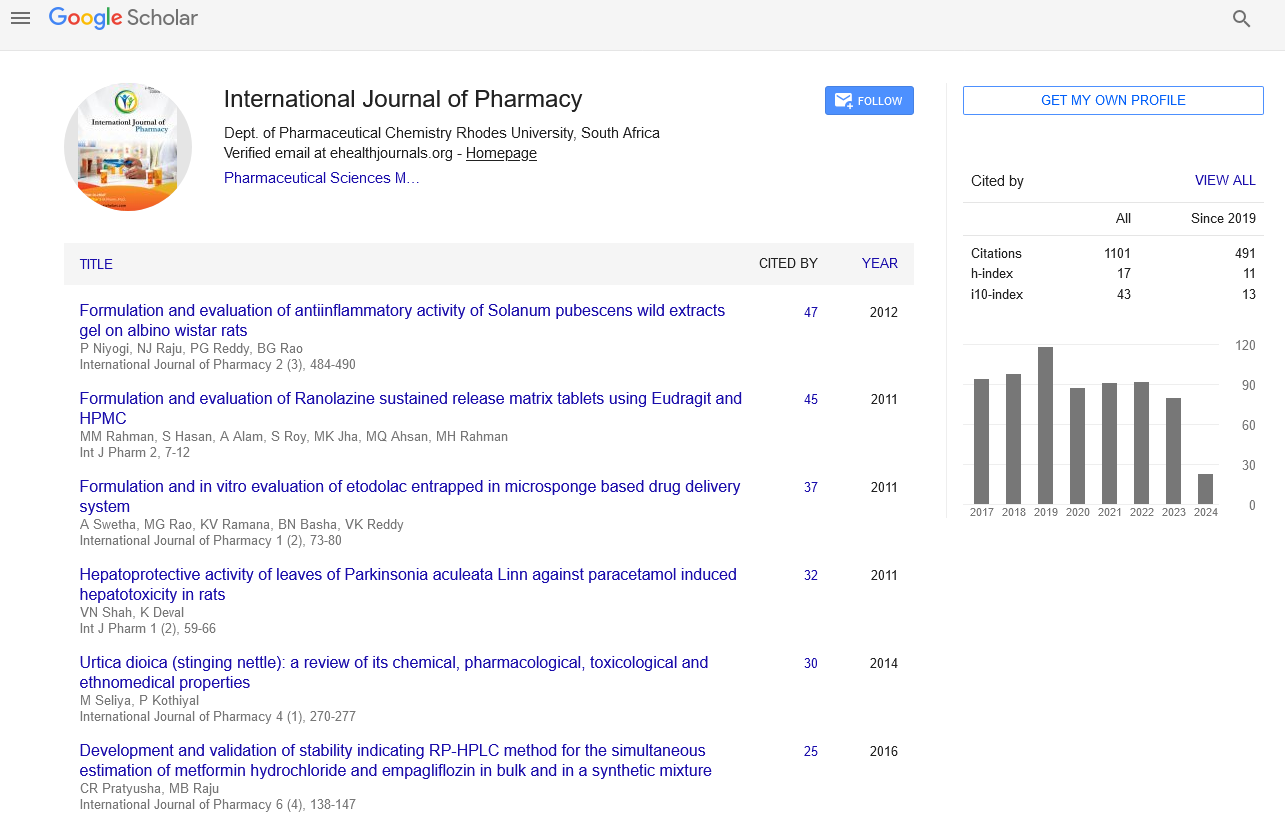
Google scholar citation report
Citations : 1101
International Journal of Pharmacy received 1101 citations as per google scholar report
International Journal of Pharmacy peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- HINARI
- Index Copernicus
- Google Scholar
- The Global Impact Factor (GIF)
- Polish Scholarly Bibliography (PBN)
- Cosmos IF
- Open Academic Journals Index (OAJI)
- Directory of Research Journal Indexing (DRJI)
- EBSCO A-Z
- OCLC- WorldCat
- MIAR
- International committee of medical journals editors (ICMJE)
- Scientific Indexing Services (SIS)
- Scientific Journal Impact Factor (SJIF)
- Euro Pub
- Eurasian Scientific Journal Index
- Root indexing
- International Institute of Organized Research
- InfoBase Index
- International Innovative Journal Impact Factor
- J-Gate