HTML
Opinion Article - (2023) Volume 13, Issue 3
Development of High Risk Pulmonary Embolism in Dyspnea
Zeya Sew**Correspondence: Zeya Sew, Department of Pharmacy, University of Cairo, Giza City, Giza, Egypt, Email:
Received: 03-Apr-2023, Manuscript No. IJP-23-100974; Editor assigned: 05-Apr-2023, Pre QC No. IJP-23-100974(PQ); Reviewed: 24-Apr-2023, QC No. IJP-23-100974; Revised: 03-May-2023, Manuscript No. IJP-23-100974(R); Published: 12-May-2023, DOI: 10.37532/2249-1848.2023.13(3).52
Description
High risk Pulmonary Embolism (PE) in dyspnea is a critical medical condition that requires prompt recognition and intervention. Pulmonary embolism refers to the blockage of one or more pulmonary arteries by a blood clot, usually originating from the deep veins of the legs. It is a potentially life-threatening condition that can lead to severe complications, including death. Dyspnea, or difficulty in breathing, is a common symptom of PE, which occurs when a blood clot forms in the pulmonary arteries, obstructing blood flow to the lungs. When a patient presents with dyspnea and is suspected of having a high-risk PE, it signifies a potentially life- threatening situation. The identification and prompt management of high-risk PE in dyspnea are crucial due to the associated risks of hemodynamic instability, right heart failure, and even death. When a patient presents with dyspnea (shortness of breath) and is suspected of having a high-risk PE, it indicates a severe obstruction in the pulmonary arteries.
This obstruction can result in significant impairment of blood flow to the lungs, causing an inadequate oxygen supply to the body's vital organs. It is essential to recognize and manage this condition promptly to minimize morbidity and mortality. Clinical evaluation plays a crucial role in assessing the severity of PE in dyspnea. Healthcare professionals should evaluate the patient's clinical history, symptoms, vital signs, and perform a thorough physical examination. Symptoms such as sudden onset dyspnea, pleuritic chest pain (sharp chest pain worsened by breathing), hemoptysis (coughing up blood), and signs of circulatory collapse should raise suspicion for high-risk PE. This may involve administering supplemental oxygen, initiating intravenous fluids, and considering vasopressor support to maintain blood pressure.
Risk stratification tools, such as the Pulmonary Embolism Severity Index (PESI) and the simplified PESI (sPESI), can aid in assessing the severity and prognosis of PE. These tools consider various factors such as age, comorbidities, vital signs, and laboratory findings to classify patients into different risk categories. High-risk PE is characterized by hemodynamic instability, indicating a significant obstruction to blood flow. Once a high-risk PE is suspected, immediate management is crucial. Hemodynamically unstable patients require prompt resuscitation and stabilization.
In some cases, Cardiopulmonary Resuscitation (CPR) may be necessary. Anticoagulation therapy is a key stone in the management of PE. It aims to prevent further clot formation and facilitate the body's natural clot- dissolving mechanisms. The mainstay of anticoagulation is the use of parenteral anticoagulants such as unfractionated heparin or low- molecular-weight heparin. Thrombolytic therapy, which involves the use of clot-dissolving medications, may be considered in patients with hemodynamic compromise or extensive clot burden. Invasive interventions, such as catheter-directed thrombolysis or surgical embolectomy, may be necessary in select cases when there is a high risk of morbidity or mortality despite anticoagulation. These interventions aim to directly remove or dissolve the blood clot causing the obstruction in the pulmonary arteries. Close monitoring of the patient's clinical status, including vital signs, oxygenation, and laboratory values, is crucial throughout the management process. Serial imaging studies, such as Computed Tomography Pulmonary Angiography (CTPA), can help assess the response to treatment and identify any complications.
Conclusion
In conclusion, high-risk pulmonary embolism in dyspnea is a severe and potentially life-threatening condition. Prompt recognition, risk stratification, and immediate management are crucial to optimize patient outcomes. Collaboration between healthcare providers from various specialties, including emergency medicine, cardiology, and critical care, is often necessary for the comprehensive management of these complex cases.
Manuscript Submission
Submit your manuscript at Online Submission System
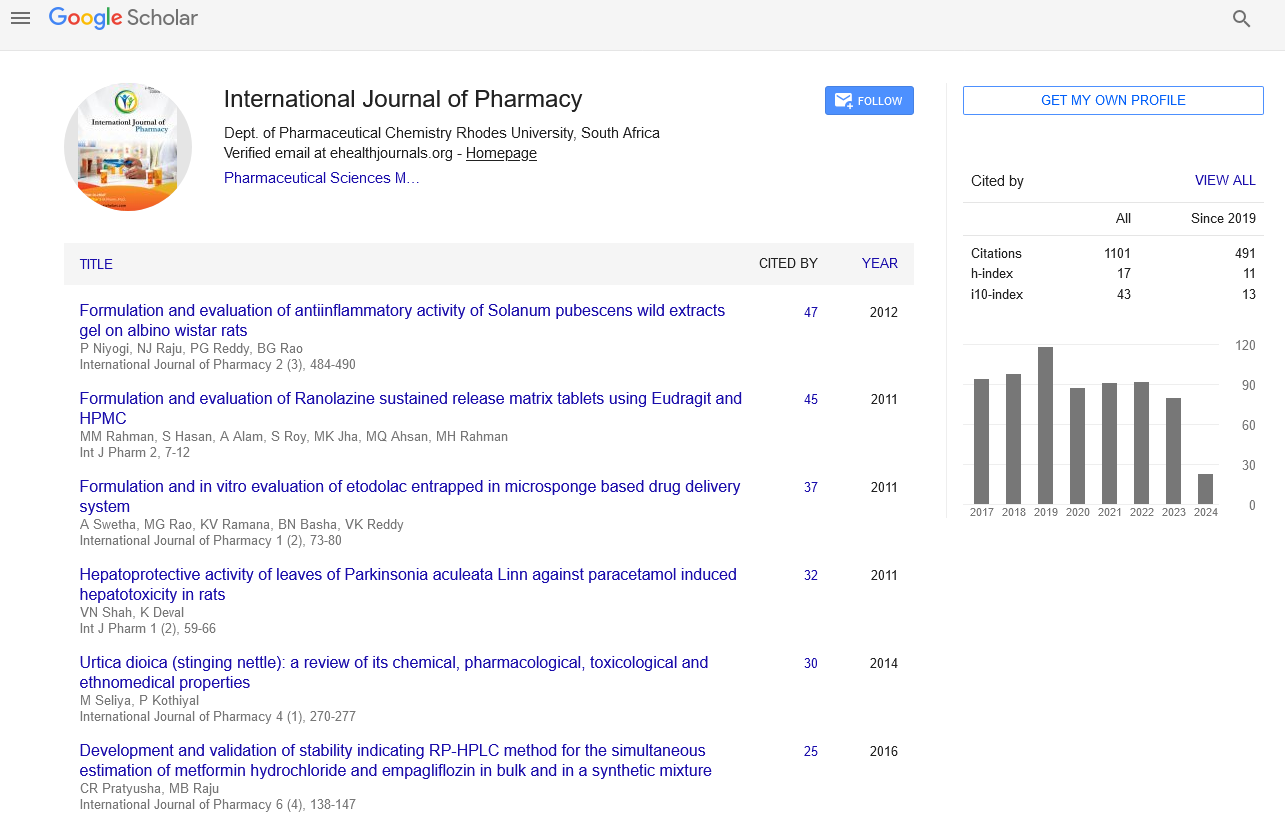
Google scholar citation report
Citations : 1101
International Journal of Pharmacy received 1101 citations as per google scholar report
International Journal of Pharmacy peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- HINARI
- Index Copernicus
- Google Scholar
- The Global Impact Factor (GIF)
- Polish Scholarly Bibliography (PBN)
- Cosmos IF
- Open Academic Journals Index (OAJI)
- Directory of Research Journal Indexing (DRJI)
- EBSCO A-Z
- OCLC- WorldCat
- MIAR
- International committee of medical journals editors (ICMJE)
- Scientific Indexing Services (SIS)
- Scientific Journal Impact Factor (SJIF)
- Euro Pub
- Eurasian Scientific Journal Index
- Root indexing
- International Institute of Organized Research
- InfoBase Index
- International Innovative Journal Impact Factor
- J-Gate