HTML
Short Communication - (2023) Volume 13, Issue 6
Managing Atrial Fibrillation Pharmaceutical Experiences: Drug Therapy vs. Interventional Treatment
Leonardo Giovanni**Correspondence: Leonardo Giovanni, Department of Pharmacy, University of Milan, Milan, Italy, Email:
Received: 19-Oct-2023, Manuscript No. IJP-23-118926; Editor assigned: 23-Oct-2023, Pre QC No. IJP-23-118926 (PQ); , QC No. IJP-23-118926; Revised: 20-Nov-2023, Manuscript No. IJP-23-118926 (R); Published: 30-Nov-2023, DOI: 10.37532/2249-1848.2023.13(6).80
About the Study
Despite a current estimated rate between 2%-4%, Atrial Fibrillation (AF) is the most common heart disease in adult patients worldwide. According to the 2020 European Society of Cardiology (ESC) Guidelines for the Diagnosis and Management of Atrial Fibrillation, a 2.3-fold increase over the next decade is expected due to increased lifespan in the general population and a more aggressive search for neglected AF. One in every three Europeans over the age of 55 will develop AF in their lifetime, applying immense pressure on our health-care systems. AFrelated consequences include a 1.5-3.5-fold increase in death, stroke (20%-30% of all ischemic strokes), and heart failure (20%- 30% of AF patients), cognitive deterioration, and dementia (hazard ratio 1.4-1.6, regardless of stroke) [1-2].
More than 60% of AF patients have a reduced quality of life, necessitating medication or ablation treatment, and the annual hospitalization rate ranges from 10% to 40%, resulting in significant costs in our health-care budgets. In 2020, a study on actual health care expenditure after Pleth Variability Index (PVI) was published, revealing considerable cost-savings on postinterventional inpatient and outpatient expenditures, as well as a reduction in days of sick leave in a PVI-population [3-5]. The new long-term study of an extended Upper Austrian cohort attempted to broaden the scope by comparing healthcare spending, results, and mortality of non-PVI medication therapy versus a PVI-based treatment plan. In recent years, growing evidence has developed that first-line PVI operations employing various ablation techniques can dramatically improve results [6].
In previous years, the research cohort of PVI patients was primarily second-line PVI, according to prior AF Guidelines, and may have only included first-line patients in recent years [7]. As a result, the study's treatment procedures may not represent the most recent standards where early rhythm control has been found to be beneficial. PVI patients in our cohort were primarily treated with Radio Frequency CA (RFCA), as cryoballoon technology. only became available after 2010. Later years, the number of patients treated with cryoballoons grew as this became the primary technology at one of the three upper. Austrian ablation centers. In our patient group, the ratio of RFCA to cryoballoon is roughly twothirds to one-third [8-9].
More sophisticated RFCA catheters with force-management reached the market in 2011 and were the leading technology as of 2012, with further technological advancements over the years. To the best of our knowledge, this is the empirical study comparing a PVI-based strategy vs. medication therapy (non-PVI) in AF patients based on actual hospital and outpatient health care expenses [10-11]. It observes a short-run rise in health-care spending of approximately €4100 per year, which levels off at €2200 per year after fhfAF. Because most PVI operations are conducted within two years of the initial AF hospitalization, the short-term rise in expenses primarily reflects ablation procedure costs, which are computed in Austria with €9873 (MEL-coding DE060) [12-13].
The higher cardio version rate in both time periods, as well as a higher rate of pacemaker implantation in the long run, is a second driver of expenditures in the PVI group. The third component of greater PVI expenses is an increase in outpatient health care. The greater short-term drug costs in PVI patients balance out in the long run. In terms of important cardio-vascular disease medication, the PVI-group had significantly greater prescription likelihood for anticoagulants, antiarrhythmic, and lipid-lowering medications. Higher outpatient expenses, as well as increased use of these relevant drugs, may explain some of the PVI group's reduced death rate. Of fact, all-cause mortality is the most difficult and crucial outcome in medical interventions [14].
A PVI-based treatment plan results in increased healthcare expenditures compared to pharmacological therapy alone (non-PVI) during short and long-term periods, according to an analysis of 2026 PSM patients out of 21,791 individuals identified by their fhfAF from 2005 to 2018. The majority of this cost excess is due to the PVI procedures. Thus, more effective and efficient ways are. required to not only reduce intervention costs, but also to avoid repeat procedures. Render AAD use after PVI unnecessary [15].
It can demonstrate a considerable reduction in all-cause mortality in patients treated with a PVI-based strategy, which we ascribe in part to the PVI process itself, stricter risk factor assessment and treatment, a thorough medical work-up, and more stringent medical care in PVI patients.
References
- Hindricks G, Potpara T, Dagres N, et al. Eur Heart J. 2021;42(5):373-498.
[Crossref] [Google Scholar] [PubMed]
- Martinek M, Pürerfellner H, Blessberger H, et al. Europace. 2020;22(4):576-583.
[Crossref] [Google Scholar] [PubMed]
- Wazni OM, Dandamudi G, Sood N, et al. N Engl J Med. 2021;384(4):316-324.
[Crossref] [Google Scholar] [PubMed]
- Rovaris G, Ciconte G, Schiavone M, et al. EP Europace. 2021;23:1380-1390.
[Crossref] [Google Scholar] [PubMed]
- Kirchhof P, Camm AJ, Goette A, et al. N Engl J Med. 2020;383:1305-1316.
[Crossref] [Google Scholar] [PubMed]
- Friedman DJ, Field ME, Rahman M, et al. Heart Rhythm O2. 2021;2:28-36. .
[Crossref] [Google Scholar] [PubMed]
- Gupta D, Vijgen J, De Potter T, et al. Heart. 2021;107:1296-1302.
[Crossref] [Google Scholar] [PubMed]
- Kirchhof P, Benussi S, Kotecha D, et al. Eur Heart J. 2016;37:2893-2962.
[Crossref] [Google Scholar] [PubMed]
- Chun KJ, Brugada J, Elvan A, et al. J Am Heart Assoc. 2017;6:e006043.
[Crossref] [Google Scholar] [PubMed]
- Murray MI, Jofre-Bonet M, Naci H, et al. J Atr Fibrillation. 2018;11:2069.
[Crossref] [Google Scholar] [PubMed]
- Saliba W, Schliamser JE, Lavi I, et al. Heart Rhythm. 2017;14:635-642.
[Crossref] [Google Scholar] [PubMed]
- Packer DL, Mark DB, Robb RA, et al. JAMA. 2019;321:1261-1274.
[Crossref] [Google Scholar] [PubMed]
- Singh BN. Cardiovasc Res. 1972;6(2):109-119.
[Crossref] [Google Scholar] [PubMed]
- Vaughan Williams EM. J Clin Pharmacol. 1984;24:129-147.
[Crossref] [Google Scholar] [PubMed]
- Echt DS, Liebson PR, Mitchell LB, et al. N Engl J Med. 1991;324(12):781-788.
[CrossRef] [Google Scholar] [PubMed]
Manuscript Submission
Submit your manuscript at Online Submission System
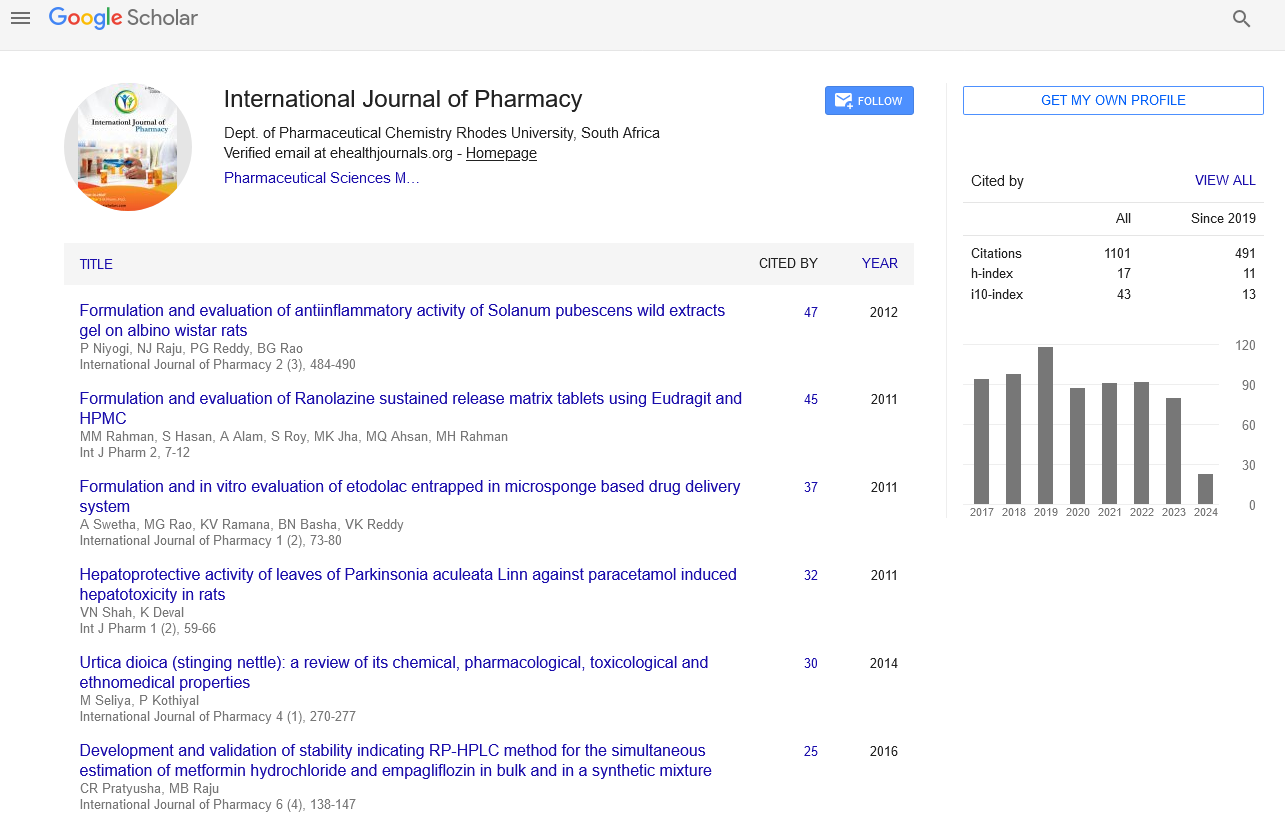
Google scholar citation report
Citations : 1101
International Journal of Pharmacy received 1101 citations as per google scholar report
International Journal of Pharmacy peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- HINARI
- Index Copernicus
- Google Scholar
- The Global Impact Factor (GIF)
- Polish Scholarly Bibliography (PBN)
- Cosmos IF
- Open Academic Journals Index (OAJI)
- Directory of Research Journal Indexing (DRJI)
- EBSCO A-Z
- OCLC- WorldCat
- MIAR
- International committee of medical journals editors (ICMJE)
- Scientific Indexing Services (SIS)
- Scientific Journal Impact Factor (SJIF)
- Euro Pub
- Eurasian Scientific Journal Index
- Root indexing
- International Institute of Organized Research
- InfoBase Index
- International Innovative Journal Impact Factor
- J-Gate