HTML
Commentary - (2024) Volume 14, Issue 3
The Role of Medications and its Insights in Diabetes Management
Carmen Rose**Correspondence: Carmen Rose, Department of Pharmacy, University of Sydney, Sydney, Australia, Email:
Received: 18-Apr-2024, Manuscript No. IJP-24-137595; Editor assigned: 22-Apr-2024, Pre QC No. IJP-24-137595 (PQ); Reviewed: 06-May-2024, QC No. IJP-24-137595; Revised: 14-May-2024, Manuscript No. IJP-24-137595 (R); Published: 22-May-2024, DOI: 10.37522/2249-1848.2024.14(3).108
About the Study
Diabetes is a chronic disease that affects how body turns food into energy. It involves problems with the hormone insulin, which is essential for converting glucose into energy. There are two main types of diabetes: Type 1, where the body doesn't produce insulin, and Type 2, where the body doesn't use insulin properly. Managing diabetes often requires medications to help control blood sugar levels.
Insulin therapy
Insulin therapy is vital for people with Type 1 diabetes and often necessary for those with Type 2 diabetes as their condition progresses. Insulin helps glucose enter the cells for energy. There are several types of insulin based on how quickly and how long they work.
Rapid-acting insulin: Starts to work within 15 minutes and lasts for 2-4 hours (e.g., lispro, as part).
Short-acting insulin: Takes about 30 minutes to work and lasts 3-6 hours (e.g., regular insulin).
Intermediate-acting insulin: Starts to work in 2-4 hours and lasts 12-18 hours (e.g., NPH insulin).
Long-acting insulin: Takes several hours to start working and lasts up to 24 hours or longer (e.g., glargine, detemir).
Insulin is typically administered through injections or an insulin pump, which can deliver a continuous supply.
Oral medications for type 2 diabetes
Oral medications are primarily used to treat Type 2 diabetes. They help manage blood glucose levels through different mechanisms.
Metformin: This is usually the first medication prescribed. It reduces glucose production in the liver and improves insulin sensitivity.
Sulfonylureas: These stimulate the pancreas to produce more insulin (e.g., glipizide, glyburide).
Meglitinides: Similar to sulfonylureas, they increase insulin production but act faster and for a shorter period (e.g., repaglinide, nateglinide).
Thiazolidinediones (TZDs): They make the body's tissues more sensitive to insulin (e.g., pioglitazone, rosiglitazone). However, they have been associated with side effects like weight gain and an increased risk of heart disease.
DPP-4 inhibitors: These help increase insulin production and decrease glucose production (e.g., sitagliptin, saxagliptin).
SGLT2 inhibitors: They help the kidneys remove glucose from the bloodstream (e.g., canagliflozin, dapagliflozin). They also provide cardiovascular and renal benefits.
Alpha-glucosidase inhibitors: These slow down the digestion of carbohydrates in the intestines (e.g., acarbose, miglitol).
Injectable medications
Aside from insulin, other injectable medications are used to treat diabetes.
GLP-1 receptor agonists: These resemble the incretin hormone, which increases insulin secretion in response to meals and slows gastric emptying, helping to lower blood sugar levels (e.g., exenatide, liraglutide). They also promote weight loss, which is beneficial for many Type 2 diabetes patients.
Amylin analogs: These are used alongside insulin in people with Type 1 or Type 2 diabetes to control blood sugar levels after meals by slowing gastric emptying and reducing glucagon secretion (e.g., pramlintide).
Combination therapies
Combining medications is often more effective than using a single medication alone. For example, a patient might take metformin along with a sulfonylurea or an SGLT2 inhibitor. This approach can help achieve better glucose control by targeting different pathways involved in blood sugar regulation.
Future and emerging treatments
Research into diabetes medications continues, with new drugs and technologies on the horizon. For instance, closed-loop insulin delivery systems (artificial pancreas) are being developed to automatically adjust insulin levels in response to blood glucose readings, offering better control and convenience. Additionally, gene therapy and beta-cell replacement therapy are being explored as potential cures.
Managing Side Effects and Risks
All medications come with potential side effects. Common side effects of diabetes medications can include hypoglycaemia (low blood sugar), gastrointestinal issues, weight gain, and increased risk of infections. Patients must work closely with their healthcare provider to monitor their condition, adjust dosages, and manage any adverse effects.
Conclusion
Diabetes management requires a personalized approach, considering the specific needs and conditions of each patient. With a variety of medications available, from insulin to oral drugs and injectable, patients have many options to maintain good glucose control. Ongoing advancements in diabetes research promise even more effective and convenient treatments in the future, improving the quality of life for those living with this chronic condition.Manuscript Submission
Submit your manuscript at Online Submission System
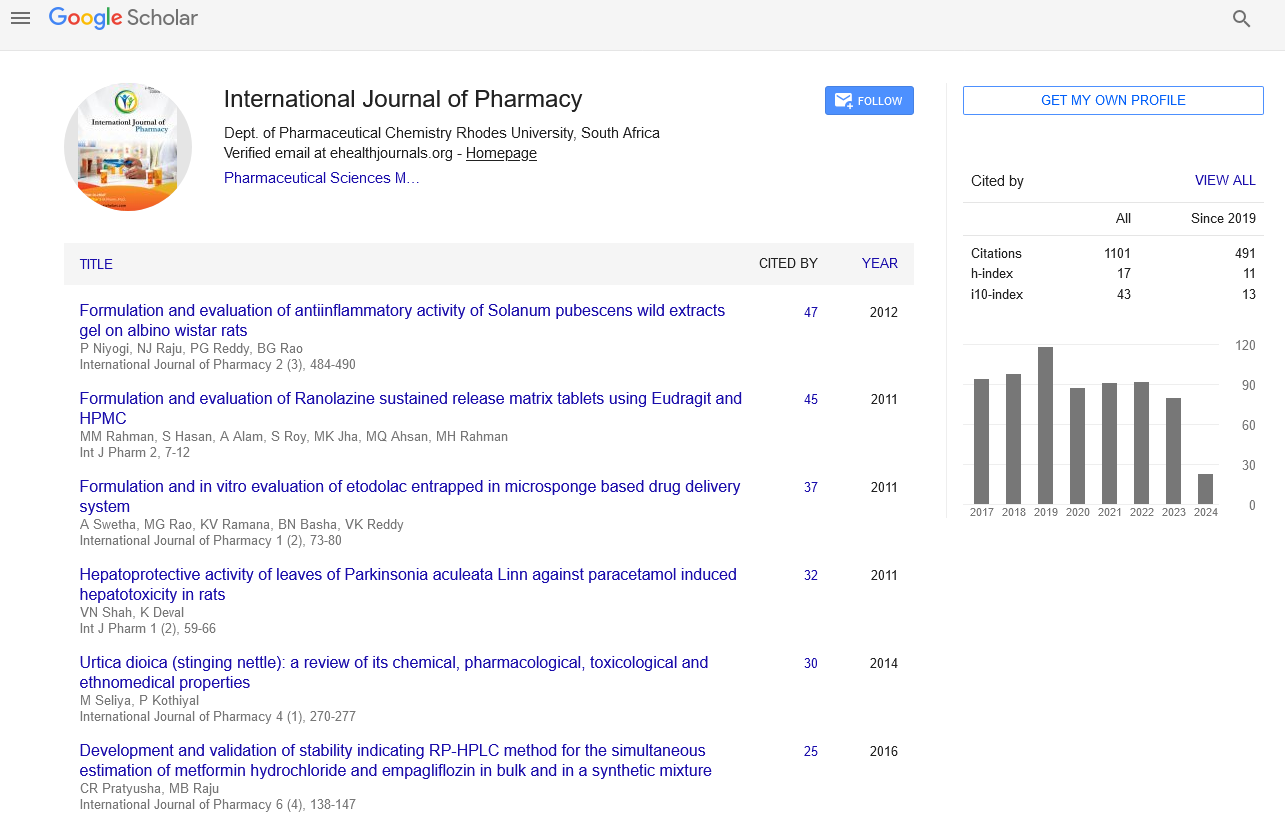
Google scholar citation report
Citations : 1101
International Journal of Pharmacy received 1101 citations as per google scholar report
International Journal of Pharmacy peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- HINARI
- Index Copernicus
- Google Scholar
- The Global Impact Factor (GIF)
- Polish Scholarly Bibliography (PBN)
- Cosmos IF
- Open Academic Journals Index (OAJI)
- Directory of Research Journal Indexing (DRJI)
- EBSCO A-Z
- OCLC- WorldCat
- MIAR
- International committee of medical journals editors (ICMJE)
- Scientific Indexing Services (SIS)
- Scientific Journal Impact Factor (SJIF)
- Euro Pub
- Eurasian Scientific Journal Index
- Root indexing
- International Institute of Organized Research
- InfoBase Index
- International Innovative Journal Impact Factor
- J-Gate